Beginning of screening of 58 neonatal metabolic disorders in Iran (Part II - Generalities)

Beginning of screening of 58 neonatal metabolic disorders in Iran (Part II - Generalities)
Following the discussion of the first part, it was determined that timely diagnosis of a metabolic disease during the process of screening infants will have the following advantages:
- Carrying out appropriate and timely treatment measures for the desired baby
- Provide the necessary genetic advice for the baby and parents
- Consider correct diagnoses of pregnancy during future pregnancies
Disorders that are considered in the primary screening of infants (screening) should have the following criteria:
1- The prevalence of the disease in the study population is such that screening seems justified.
2- Finally, the desired disease is well defined if not treated.
3- It should be clearly defined what importance and contribution of non-treatment will be in the mortality or morbidity of the baby.
4- There should be an effective treatment for the disease in such a way that it can reduce or prevent the adverse effects and consequences of the disease.
5. The test is safe, simple, and sensitive enough to detect babies with the disease.
6- For cases where the screening test is positive, there is a suitable confirmation test.
7- The cost price for testing, treatment and prevention of the consequences of the disease should be lower than the cost of managing the untreated cases.
Some diseases meet all of the above criteria, such as phenylketonuria (PKU), which is common in screening programs with a prevalence of 1 in 10,000 in all countries.
If left untreated, PKU can cause the baby to become mentally retarded and even require long-term care in a mental retardation center, thus imposing a large financial cost on the family.
But early detection and early nutritional interventions (such as eliminating phenylalanine from the diet) have very good consequences, and the sufferer may have a normal life.
Screening tests are inexpensive and accurate, with the measurement of a substance called phenylalanine in a dried blood stain on filter paper.
In addition, it is easily possible to perform diagnostic tests in many laboratories.
In general, metabolic disorders fall into three diagnostic groups:
1. Disorders in which the body's metabolism (in order to produce energy) is disrupted, resulting in permanent, progressive, unrelated manifestations of simultaneous events. These disorders are not related to the food consumed. Such as lysosomal disorders, peroximal disorders and transmission or intracellular processes.
2 - Disorders that the problem is related to intermediate metabolic pathways and causes the accumulation (accumulation) of toxic substances (toxic) in the body (because these substances can not be consumed naturally). Such as metabolic disorders of amino acids
3- Disorders caused by lack of energy production or lack of energy consumption in the liver, heart, muscles and brain. These diseases include congenital lactic acidemias, fatty acid oxidation defects, gluconeogenesis defects, and mitochondrial respiratory chain disorders.
Most inherited disorders are autosomal recessive, ie:
That is, a copy of the defective gene must be passed from each parent to the patient for the disease to occur.
- It is observed in girls and boys in the same proportion,
- Consanguineous marriage is more common in consanguineous marriages.
In communities with high intra-marital coefficients (Inbreeding coefficient), it is possible for a person to inherit a pair of alleles from their ancestor through
High parents (like Iran) are more common,
- Parents of defective gene carriers have a 25% chance of having a sick baby.
(Except for the lack of ornitine trans carbamylase, which is one of the disorders of the urea cycle and its gene is located on the X chromosome and
Deficiency of this enzyme is a sex-dependent disease.
In one-third of children with metabolic diseases caused by the accumulation of toxins or a defect in energy production, the disease manifests itself with a delay (late onset), meaning that the baby appears healthy at birth and the symptoms usually appear later. They occur from a year or later.
Symptoms usually include viral infections, fever, or severe diarrhea. Because in these conditions, the rate of breakdown of stored cellular and tissue proteins increases and the symptoms of these diseases accelerate. These attacks can improve on their own or require intensive care. These attacks may occur after overeating (eg, Eid and holidays).
The concept of primary and secondary biomarkers in neonatal screening
Biomarkers are molecules that are naturally present in body fluids and can be used to measure normal biological processes, disease status, or response to treatment. Primary biomarkers are metabolites that, under the biochemical pathway of a specific disease process, change in value and are diagnosed. Secondary biomarkers, meanwhile, are substances whose changes increase the risk of a metabolic disease. These markers are mostly shown as a ratio between analytes.
General clinical symptoms of disorders
Clinical diagnosis of metabolic diseases is very difficult because their symptoms are non-specific and can be seen in other diseases. Babies with metabolic diseases are usually normal at birth. It is often a sign of a non-specific inherited metabolic disease and is similar to a blood infection or congenital heart disease. Signs and symptoms include drowsiness, nausea, seizures, and vomiting, and may appear as early as a few hours after birth. But they usually appear late in the first week when the baby is breastfed enough. Newborn metabolic diseases, if left untreated, can lead to mental retardation, severe mental disorders, and even infant death.
1- Demonstrations: Generally occur in the form of weakness, lethargy and coma. In this group, there is usually an asymptomatic period, the duration of which varies depending on the type of disorder. After a period of asymptomatic symptoms such as anorexia, lethargy and decreased level of consciousness appear, followed by disturbances in respiration and heart rhythm as the heart rate decreases. Hypothermia (decrease in body temperature), tremor (potential), muscle cuts, and eventually coma occur with normal or severe muscle contractions.
2. Seizures: Seizures in isolation (= the only symptom) are very rare in metabolic diseases and can only be seen in seizures associated with pyridoxine deficiency (vitamin B6), folic acid, biotin, and congenital magnesium malabsorption, all of which are treatable. In other metabolic diseases, however, seizures are often associated with hypoglycemia (= low blood sugar), decreased level of consciousness, and coma.
3- Muscle: It occurs in various forms such as muscle weakness and muscle cramps.
4 - Dysmorphism and malformations (malformation and anomaly): Some metabolic diseases with facial dysmorphism with anomalies.
5 - Hepatic manifestations: Most often occur in the form of liver failure, the symptoms of which include jaundice, increased liver enzymes, death of liver cells, hypoglycemia and accumulation of fluid in the abdominal cavity.
6 - Cardiac manifestations: Heart enlargement, which is often accompanied by muscle weakness, is mainly seen in fatty acid disorders. Sometimes heart symptoms are seen only as arrhythmias or disorders of the cardiovascular system.
7- Hyper-ammonia (increase in blood ammonia): Acute neurological disorders are the main picture of ammonia increase and at the top of its differential diagnoses are cyclic urea and organic acid disorders. Hyperammonemia is the key to diagnosing some diseases. For example, in the deficiency of the enzymes pyruvate carboxylase and glutaric acid of type 2, hyperammonemia may appear in the first 24 hours of life. In cyclic urea disorders, however, ammonia usually increases after the first 24 hours after feeding. It should be noted that hyperammonemia is not specific to metabolic diseases, it may also be seen in premature infants, infants with congenital herpes, and liver dysfunction.
8- Metabolic acidosis: Acidosis is a condition in which the pH of the blood decreases to less than 7.35. This condition can be of respiratory or metabolic origin. Metabolic acidosis (caused by an increase in other acids in the blood (lactic acid, pyruvic acid, etc.) is a common finding in many metabolic diseases.
9- Hypoglycemia (hypoglycemia): In most disorders of protein, carbohydrate and fatty acid metabolism, hypoglycemia is observed, at the top of which is GSD (Glycogen Storage Disease). The presence or absence of estrogenic compounds in the blood helps to differentiate these diseases.
10 - Eye failure: such as cataracts and glaucoma
11- Sudden infant death syndrome
12- Gastrointestinal manifestations: anorexia, vomiting, diarrhea and malabsorption
Some diseases have specific symptoms, such as discoloration of the lens of the eye and blood clots, which are specific to homocysteinuria, but others are non-specific symptoms, such as liver enlargement, seizures, and mental retardation.
The spread of diseases
In general, these diseases are divided into the following categories in terms of prevalence:
1- Common: such as favism (or deficiency of G6PD enzyme) with a prevalence of 1: 100
2 - Relatively common but still rare (relatively more common but still rare): such as hypothyroidism with a prevalence of 1: 4000, phenylketonuria with a prevalence between 1: 6000 to 1: 10000 (in Iran the prevalence is 1: 5000), disorders Urea cycle with a prevalence of 1: 8000, congenital adrenal gland congestion 1: 10000 to 1: 18000 and the total incidence of organic acids 1: 20000
3- Rare: such as galactosemia with a prevalence of 1: 40,000 to 1: 60,000, deficiency of the enzyme biotinidase with a prevalence of 1: 60,000 and sickle cell anemia 1: 40,000
4- Very rare: such as urinary syrup in maple syrup with a prevalence of 1: 180000 and homocytinuria with a prevalence of 1: 250000 and a disorder in reabsorption of carnitine 1: 250000
5 - Extremely rare: less than 1: 100,000
Note: If the prevalence of a disease is 1: 1000, it indicates that the prevalence of carriers will be 1: 500.
Due to the prevalence of consanguineous marriages in Iran, as well as the high intra-marital coefficient (the probability of inheriting a pair of alleles from an ancestor through parents), approximately one in every 500 to 600 infants suffers from inherited metabolic diseases. Due to the lack of timely diagnosis, they will face severe complications in the future.
- The total rate of consanguineous marriage is 38.6% and the coefficient of intermarriage in Iran is 0.0185
- Intra-marital coefficient in Canada 0.00004 to 0.0008
- Intra-marital coefficient in the United States 0.001 to 0.005
- Intra-marital coefficient in Saudi Arabia 0.024
Thus, in general, congenital metabolic disorders alone are rare diseases, but are generally relatively common.
treatment
The main purpose of treatment in these diseases is the following:
- Trying to prevent the accumulation of toxic substances in the body and also to compensate for the metabolic substance that is deficient.
- Withdrawal of toxins accumulated in the body by methods such as fluid administration (to compensate for the lack of breastfeeding, increase fluid flow and ensure effective excretion of toxic metabolites), blood transfusion, dialysis or hemodialysis
- Treatment with vitamins as therapeutic cofactors in cases of deficiency and deficiency of related groups and increased metabolism
- Prescribe high doses of glucose to reduce the consumption of proteins and fatty acids
- Enzyme therapy, gene therapy
Dr. Sarang Younesi *, Dr. Mohammad Mehdi Taheri Amin *, Dr. Pourandokht Saadati **
* Doctors of Clinical Laboratory Science
** Clinical and descriptive pathology specialist
Nilo Lab
-
 Screening of 58 neonatal metabolic disorders in Iran (Part 12 - Review of Urinary Tract Urinary Disease or MSUD)
Screening of 58 neonatal metabolic disorders in Iran (Part 12 - Review of Urinary Tract Urinary Disease or MSUD) -
 Screening of 58 neonatal metabolic disorders in Iran (Part 11 - Review of Phenylketonuria)
Screening of 58 neonatal metabolic disorders in Iran (Part 11 - Review of Phenylketonuria) -
 Screening of 58 neonatal metabolic disorders in Iran (Part 10 - Report of an infant with ischemic ischemia)
Screening of 58 neonatal metabolic disorders in Iran (Part 10 - Report of an infant with ischemic ischemia) -
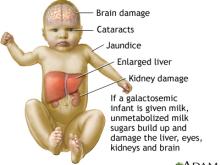 Screening of 58 neonatal metabolic disorders in Iran (Part 9 - Galactosomia)
Screening of 58 neonatal metabolic disorders in Iran (Part 9 - Galactosomia) -
 Screening of 58 neonatal metabolic disorders in Iran (Part 8 - Congenital adrenal insufficiency)
Screening of 58 neonatal metabolic disorders in Iran (Part 8 - Congenital adrenal insufficiency) -
 Screening of 58 neonatal metabolic disorders in Iran (Part 7 - Biotinidase deficiency)
Screening of 58 neonatal metabolic disorders in Iran (Part 7 - Biotinidase deficiency) -
 Screening for 58 neonatal metabolic disorders in Iran (Part 6 - Organic Acid Disorders)
Screening for 58 neonatal metabolic disorders in Iran (Part 6 - Organic Acid Disorders) -
 Screening for 58 neonatal metabolic disorders in Iran (Part 5 - Fatty Acid Disorders)
Screening for 58 neonatal metabolic disorders in Iran (Part 5 - Fatty Acid Disorders) -
 Screening of 58 neonatal metabolic disorders in Iran (Part IV - Amino Acid Disorders)
Screening of 58 neonatal metabolic disorders in Iran (Part IV - Amino Acid Disorders) -
 Screening of 58 neonatal metabolic disorders in Iran (Part III - Urea Production Cycle Disorders)
Screening of 58 neonatal metabolic disorders in Iran (Part III - Urea Production Cycle Disorders)

