Metabolic emergencies in newborns

Metabolic emergencies in newborns
Collected by: Ms. Bahareh Yazdani - Senior Laboratory Expert
Metabolic emergencies in newborns
Dr. Jason Woods, a pediatric emergency physician at Children's Hospital in Colorado, USA, generally points out that metabolic emergencies are rare in infants, and that is why the vast majority of these infants have metabolic diseases at first without They go to the hospital before they have a diagnosis.
That's why in this group of babies who are sick, we have to think about other diseases such as infection, trauma, bleeding, shock and metabolic diseases.
We must first assess all the causes, as most of these diseases have not been previously diagnosed.
After the evaluation, if you think that it is the cause of metabolic disease, the most important thing is caloric support, which means that we are sure that the patient is supported in terms of calories.
The first step is to give the patient glucose.
Dr. Woods recommends starting D10 Fluid or (Dextrose 10%) with 1.5 times the Maintenance Fluid for the patient.
In most metabolic patients, part of their metabolic pathway is impaired, and giving glucose can cause the problem to be bypassed or, in other words, eliminated.
If the baby is hypoglycemic, you can use rule 50.
Rule 50 states that for newborns, you can give 5 ml per kilogram of D10.
For multi-month-old babies, you can give 2 ml per D25 kg, and for babies and adolescents you can give 1 ml for every D50 kg.
As you know, 5 ml for each kilogram of D10 (5 × 10 becomes 50, 2 ml for each kilogram of D25 (2 × 25) becomes 50 and 1 ml for each kilogram of D10 (1 × 50) becomes 50 This law is called 50.
If the patient has acidosis and shows signs of shock and heart failure, you can give the patient a bicarbonate.
Every infant who enters the emergency department should always prioritize ABC (Airway Breathing Circulation).
Once the baby's condition is established, you can look at different possibilities.
In the United States, any newborn born is required to undergo Newborn Screening.
Usually in the first 24 hours after birth, a few drops of blood are taken from the baby's heel and sent to a laboratory. The test usually takes a week or two, depending on the state.
Therefore, if a parent goes to the emergency room and states that their baby has a metabolic disease, they are more likely to call the patient's family from the lab and answer the screening test.
If the first result of the screening is negative, the risk of metabolic disease is very, very low, but does not reach zero.
Remember that this test is a public health test and is not 100% specific and sensitive.
In addition, it cannot detect all metabolic diseases such as Glycogen Storage Disorders and Mitochondrial Disorders.
Assuming a one-week-old baby is referred to the emergency department, in what cases should we suspect metabolic diseases?
Dr. Woods says that if you have a disease that has anorexia or eating problems or a problem with your body temperature and is lethargic and doesn't look healthy and your metabolic screening response isn't ready yet, then you probably should. Think of metabolic diseases.
In this case, many experiments that are easily available in most laboratories can be performed for diagnosis.
Experiments such as measuring the levels of glucose, lactate, ammonia, uric acid and ketones.
Now let's talk about each of these tests separately.
Uric acid: If the result of this test is too far away from normal, the risk of metabolic disease is very high, but this test should not affect your emergency management.
Ammonia: Direct Neurotoxin and easily crosses the Blood Brain Barrier (BBB) because it is fat-soluble.
That's why Hyper Ammonia causes Encephalopathy in sick babies.
Sampling for ammonia measurement should be without a tourniquet and taken slowly, and after sampling should be kept on ice.
In this case, the exact answer is obtained. If the ammonia level is below µl / L50, it is normal.
But if the ammonia level is between 100 and 200, Dr. Woods says the test should be repeated, and if the level is above 200, the risk of metabolic disease is high.
Dr. Woods points out that the amount of ammonia in the blood is not very important, in fact, what usually causes nerve damage is that this hyperammonia stays in the body for a long time and is not treated.
Unfortunately, there are no definitive guidelines or protocols for treating hyperhidrosis.
But Dr. Woods says you can use dialysis if the amount of ammonia is higher than 300, even though the patient is being supported.
Now, we come to the part where we talk about the middle ground.
Most babies with hypoglycemia do not have a congenital metabolic disease, and the main reason for hypoglycemia in these babies is malnutrition.
In metabolic diseases, hypoglycemia occurs when the patient does not eat for 4-6 hours, so infants are less likely to develop hypoglycemia because they are breastfed every 2-3 hours.
Now let's talk about each of these tests separately.
That's why most of these children are diagnosed a little later.
Usually, when they get a little older and there is a gap between eating, the metabolic disease becomes apparent.
Dr. Woods points out about Glycogen Storage Disorders that if you have a disease that you think has the disease, keep in mind that most of these patients have a large liver (hepatomegaly) that is detected on a physical examination.
In these patients, if they do not eat for 4-6 hours, they will be diagnosed with hypoglycemia.
If they become hypoglycemic earlier than 4 hours, there is another reason.
As for the amount of lactate, as you know, many disorders and diseases cause high lactate.
If the lactate level is too high and the patient has Anion Gap Acidosis and there is no reason for the lactate to be high, then we can think of a metabolic disease for high lactate.
Lactate is a glycosylated product and hyperglycemia itself can cause high lactate.
Dr. Woods says Bicarbonate is not a standard treatment for acidosis unless the patient has shock and heart failure, at which time Bicarbonate can be used to treat acidosis.
If a patient has Acidosis Non Anion Gap, the risk of metabolic disease is very low. We must remember that babies usually do not make ketones unless they have metabolic disease or high lactate.
If there is even a small amount of ketones in the baby's urine, you should imagine that the patient or infant has a metabolic problem unless proven otherwise.
Dr. Woods also points to the use of Intra lipid and says that Intra lipid is used for most metabolic diseases, but we do not recommend prescribing it routinely unless your doctor tells you to.
Now the main question is who should we contact and who should we ask for help in these cases.
If you are in a large academic center or in a hospital, you can talk to Dr. Pediatrician, a specialist in metabolic and genetic diseases.
But most of us work in hospitals that do not have access to these specialists.
In these cases, Dr. Woods Jason says we can contact the nearest specialist hospital.
Most cases of neonatal disease are diseases that must be hospitalized in the PKU or NiKU department.
Dr. Woods points out that in many cases you can contact government labs and see if the Newborn Screening answer is ready, because if the answer is ready, many problems will be solved.
In the next section, Dr. Jason Woods introduces several treatment references.
The first reference is a book called vedemecom metabolicom, which is about the diagnosis and treatment of congenital metabolic diseases.
There is a free app called EVM that you can download for free, and then they point out that the New England Consortium, which is a collection of different protocols for treating metabolic diseases, you can refer to the New England Journal of Medicine and the protocol. Download them.
This episode was about diseases that have not yet been diagnosed with metabolic diseases, and their early signs are inexplicable.
Finally, Dr. Woods points out that if a patient has a specific metabolic disease and we are not particularly familiar with the disease, we can set the patient on the D10 Fluid by 1.5 times the Maintenance Fluid so that we can contact a neonatologist or metabolic disease specialist. Get more information.
And finally, the important points of this episode:
1. It is the first work of Colric Support that we can start with D10 Fluid.
Hyperimmune disease may have Respiratory Alkalosis because high levels of ammonia in the blood increase Respiratory Rate.
3. Hypoglycemia in metabolic patients occurs when the patient or infant has not eaten for 4-6 hours. Therefore, infants who are breastfed once every 2-3 hours will not show any symptoms soon.
4. If the baby has ketones, we should assume that the baby has a metabolic disease until it is proven otherwise.
5. The New England Consortium has a complete list of different protocols for treating infants with various metabolic diseases, which we can refer to for guidance.
Prepared:
Ms. Bahareh Yazdani - Master of Laboratory
In charge of neonatal screening
-
 Screening of 58 neonatal metabolic disorders in Iran (Part 12 - Review of Urinary Tract Urinary Disease or MSUD)
Screening of 58 neonatal metabolic disorders in Iran (Part 12 - Review of Urinary Tract Urinary Disease or MSUD) -
 Screening of 58 neonatal metabolic disorders in Iran (Part 11 - Review of Phenylketonuria)
Screening of 58 neonatal metabolic disorders in Iran (Part 11 - Review of Phenylketonuria) -
 Screening of 58 neonatal metabolic disorders in Iran (Part 10 - Report of an infant with ischemic ischemia)
Screening of 58 neonatal metabolic disorders in Iran (Part 10 - Report of an infant with ischemic ischemia) -
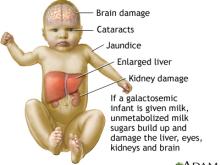 Screening of 58 neonatal metabolic disorders in Iran (Part 9 - Galactosomia)
Screening of 58 neonatal metabolic disorders in Iran (Part 9 - Galactosomia) -
 Screening of 58 neonatal metabolic disorders in Iran (Part 8 - Congenital adrenal insufficiency)
Screening of 58 neonatal metabolic disorders in Iran (Part 8 - Congenital adrenal insufficiency) -
 Screening of 58 neonatal metabolic disorders in Iran (Part 7 - Biotinidase deficiency)
Screening of 58 neonatal metabolic disorders in Iran (Part 7 - Biotinidase deficiency) -
 Screening for 58 neonatal metabolic disorders in Iran (Part 6 - Organic Acid Disorders)
Screening for 58 neonatal metabolic disorders in Iran (Part 6 - Organic Acid Disorders) -
 Screening for 58 neonatal metabolic disorders in Iran (Part 5 - Fatty Acid Disorders)
Screening for 58 neonatal metabolic disorders in Iran (Part 5 - Fatty Acid Disorders) -
 Screening of 58 neonatal metabolic disorders in Iran (Part IV - Amino Acid Disorders)
Screening of 58 neonatal metabolic disorders in Iran (Part IV - Amino Acid Disorders) -
 Screening of 58 neonatal metabolic disorders in Iran (Part III - Urea Production Cycle Disorders)
Screening of 58 neonatal metabolic disorders in Iran (Part III - Urea Production Cycle Disorders)

